22 Dec, 2023 | admin | No Comments
Revolutionizing Eye Care with AI Expertise
Dry Eye Management: Tips and Treatment Options
Dry eye syndrome is a common condition that affects millions of people worldwide. It occurs when the eyes don’t produce enough tears, or when the tears evaporate too quickly. In this blog, we’ll explore some tips and treatment options for managing dry eye syndrome.
Tips for Managing Dry Eye Syndrome
- Use a humidifier: A humidifier can add moisture to the air, which can help reduce dryness in the eyes.
- Take frequent breaks: If you work on a computer or read for long periods of time, take frequent breaks to rest your eyes.
- Blink regularly: Blinking helps spread tears evenly over the eyes, which can help prevent dryness.
- Avoid smoking and secondhand smoke: Smoking and secondhand smoke can irritate the eyes and worsen dry eye syndrome.
- Stay hydrated: Drinking plenty of water can help keep the eyes hydrated and reduce dryness.
Treatment Options for Dry Eye Syndrome
- Artificial tears: Artificial tears are over-the-counter eye drops that can help lubricate the eyes and reduce dryness.
- Prescription eye drops: If artificial tears aren’t effective, prescription eye drops may be necessary. These eye drops can help reduce inflammation and increase tear production.
- Punctal plugs: Punctal plugs are small devices that are inserted into the tear ducts to help block tear drainage, which can help keep the eyes lubricated.
- LipiFlow: LipiFlow is a treatment that uses heat and pressure to unclog the glands that produce tears, which can help improve tear production.
- Lifestyle changes: In some cases, lifestyle changes, such as reducing screen time or changing your diet, may help improve dry eye symptoms.
Conclusion
Dry eye syndrome can be a frustrating and uncomfortable condition, but there are many treatment options available to help manage the symptoms. If you’re experiencing dry eye symptoms, talk to your ophthalmologist about the best treatment options for your specific needs. With the right treatment and lifestyle changes, you can manage your symptoms and enjoy clear and comfortable vision
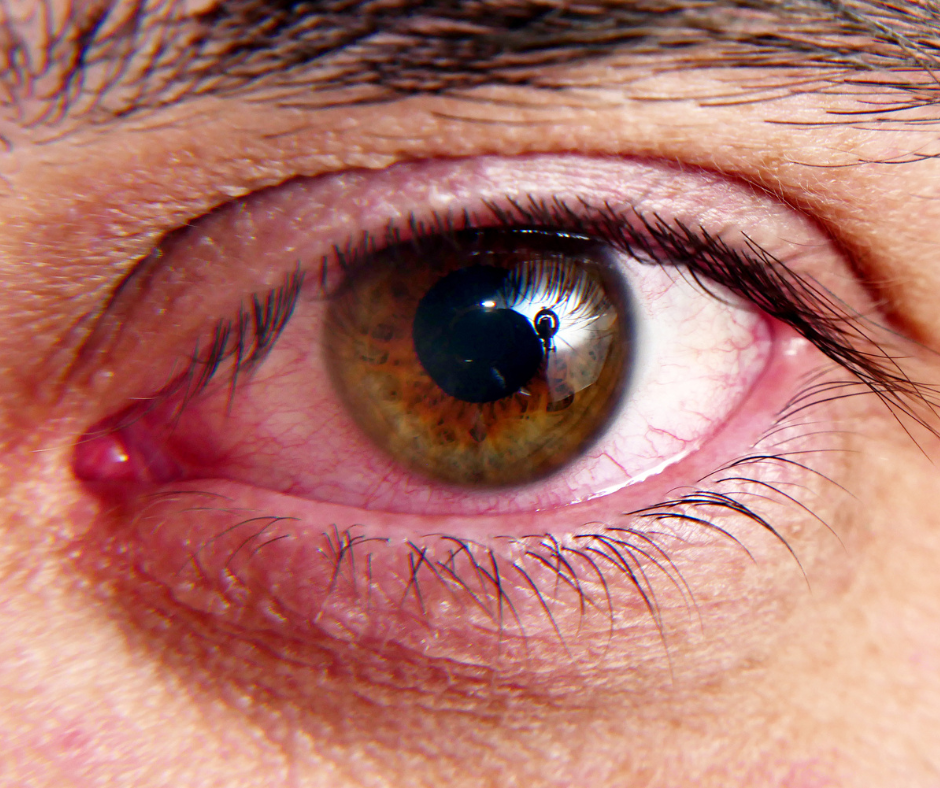
If you experience itchy, red, or watery eyes, you may be suffering from eye allergies. Eye allergies are a common condition that affects millions of people around the world. In this blog, we’ll explore the symptoms, causes, and treatment options for eye allergies.
Symptoms of Eye Allergies
The symptoms of eye allergies can vary from person to person. Some common symptoms include:
- Itchy eyes
- Red eyes
- Watery eyes
- Swollen eyes
- Sensitivity to light
- Burning or stinging sensation in the eyes
These symptoms may occur in one or both eyes and can range from mild to severe.
Causes of Eye Allergies
Eye allergies are caused by the body’s reaction to allergens, such as pollen, pet dander, dust mites, or mold spores. When these allergens come into contact with the eyes, they trigger an immune response that leads to inflammation and irritation. Eye allergies can also be caused by certain medications, cosmetics, or eye drops.
Treatment Options for Eye Allergies
The treatment for eye allergies depends on the severity of the symptoms. Mild cases of eye allergies can often be managed with over-the-counter antihistamine eye drops, which can help reduce inflammation and itchiness. Artificial tears can also help soothe dry and irritated eyes.
For more severe cases of eye allergies, prescription eye drops may be necessary. These eye drops contain stronger anti-inflammatory medication that can provide relief for more severe symptoms.
Preventing Eye Allergies
Preventing eye allergies is possible by avoiding exposure to the allergens that trigger the symptoms. If you know you’re allergic to certain substances, such as pollen, try to limit your exposure during peak allergy seasons. Keeping your home clean and free of dust and pet dander can also help reduce the risk of eye allergies.
Conclusion
Eye allergies can be uncomfortable and frustrating, but they’re also a common and treatable condition. If you’re experiencing symptoms of eye allergies, talk to your ophthalmologist about the best treatment options for your specific needs. With the right treatment, you can manage your symptoms and enjoy clear and comfortable vision.
Ocular inflammation is a common complication of eye surgery, which can be distressing for patients and may lead to further complications. Inflammation in the eye can lead to the development of macular cystoid edema, which is a condition where fluid accumulates in the macula, a part of the retina responsible for sharp, detailed vision. This can result in blurred vision, decreased visual acuity, and in severe cases, can cause permanent damage to the retina. To prevent these complications, ophthalmologists often prescribe pharmacologic therapy or surgical procedures to manage ocular inflammation. Pharmacologic therapy may involve the use of anti-inflammatory drugs, such as steroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and immunomodulatory agents. These drugs work by reducing the production of inflammatory mediators and suppressing the immune response, thereby alleviating swelling and discomfort in the eye. Less invasive surgical procedures may be used to treat ocular inflammation, such as laser photocoagulation and vitrectomy. Laser photocoagulation involves the use of a laser to seal and close off abnormal blood vessels in the retina that may be contributing to inflammation. Vitrectomy is a surgical procedure that involves the removal of the vitreous gel, a clear substance that fills the eye, and the replacement of this with a saline solution. This can help to remove any inflammatory cells and debris that may be present in the eye. It is important to note that while these treatments can be effective in managing ocular inflammation, they may also have side effects and risks associated with them. Patients should be informed of these risks and should discuss the benefits and drawbacks of each treatment option with their ophthalmologist before making a decision. Additionally, patients should be vigilant in monitoring their symptoms and reporting any changes to their ophthalmologist to ensure prompt and appropriate treatment.
25 Jun, 2021 | Bradley Naidoo | No Comments
Glaucoma, the silent thief of sight

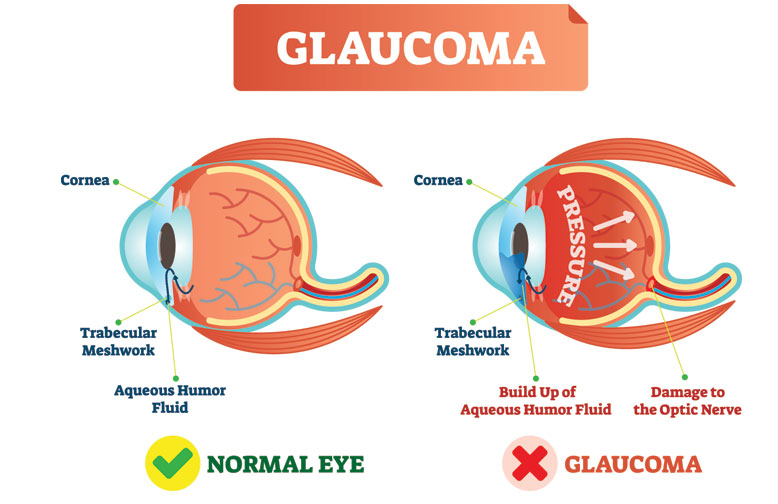
Have you ever put off an eye exam because your eyesight “seems fine”? Maybe you’ve never worried about diseases like Glaucoma because “I’m too young”? Well….This is where you may be wrong, Glaucoma is one of the leading causes of blindness in the world. In the early stages, it usually has no symptoms. Yet it is essential to catch glaucoma at this stage for the best chance of successful treatment. Glaucoma can strike as early as the age of 40. Glaucoma is a group of eye conditions that causes damage to the optic nerve. This damage is often caused by an abnormally high pressure in your eye. It can occur at any age but is more common in older adults. Many forms of Glaucoma have no warning signs. The effect is so gradual that you may not notice a change in vision until the condition is at an advanced stage.
We at PureSight Ophthalmology specialize in Glaucoma diagnosis and treatment; today we will take an in-depth look at Open-angle glaucoma as it is the most common form of the disease.
OPEN-ANGLE GLAUCOMA
Occurs when the drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked. This causes pressure in the eye to gradually increase. This pressure damages the optic nerve. It happens so slowly that you may lose vision before you’re even aware of a problem. The signs and symptoms of glaucoma vary depending on the type and stage of your condition hence the nick name of the silent thief of sight
WHO’S MOST LIKELY TO GET IT?
Your chances go up based on the following factors, Age – Your risk rises as you get older. Family history -You’re more likely to get it if other family members have it. If you have a family history of glaucoma, you should see an ophthalmologist yearly even if you do not have any symptoms. Some other conditions also raise your odds such as Diabetes, a thin cornea, high blood pressure and Near-sightedness
SYMPTOMS & TREATMENT
What Are the Symptoms? There aren’t any for quite some time and therefore regular eye exams are always recommended. Early on, you start to lose peripheral vision, the stuff you see out the side of your eyes. You may not notice it’s happening. Later, you might miss a stair while you walk or notice letters missing from words when you read. You might also have some close calls when you drive.
Open-angle Glaucoma symptoms include: Patchy blind spots in your side (peripheral) or central vision, frequently in both eyes Tunnel vision in the advanced stages

Whilst other forms of Glaucoma such as Acute angle-closure Glaucoma, you would experience the following symptoms: Severe headache; Eye pain; Nausea and vomiting; Blurred vision; Halos around lights and Eye redness.
TREATMENT OF GLAUCOMA
The damage caused to the optic nerve is irreversible and so is the vision loss or problems that follow, but you can slow Glaucoma’s progress. You do that by lowering the pressure in your eye, even if it seems normal. Generally, the more damage you have, the lower you want the pressure. Treatment for Glaucoma can be medical or surgical. Medical treatment involves the instillation of drops or tablets to reduce fluid production or increase fluid drainage. In many cases, laser therapy is indicated which, together with drops, may provide a longer period of controlled eye pressure.
GLAUCOMA SURGERY
Surgery involves the creation or implantation of a valve to control the pressure in the eye. The type of surgery your doctor recommends will depend on the type and severity of your Glaucoma and the general health of your eye. Surgery can help lower pressure when medication is insufficient. However, it cannot reverse vision loss
17 Jun, 2021 | Bradley Naidoo | No Comments
Diabetes & the Eye

Diabetes can lead to blurry vision in several ways. In some cases, it’s a minor problem that you can resolve by stabilizing your blood sugar or taking eye drops. Other times, it’s a sign of something more serious that’s worth discussing with your doctor. In fact, blurred sight is often one of the first warning signs of diabetes.
What is Diabetic Eye Disease?
Diabetic Eye Disease is a group of eye problems that can affect people with diabetes. Over time, diabetes can cause damage to your eyes that can lead to poor vision or even blindness. You can take steps to prevent diabetic eye disease or prevent existing disease from getting worse. More serious Diabetic Eye Diseases begin with blood vessel problems. The eye diseases that can threaten your sight include Diabetic Retinopathy, Diabetic Macular Oedema and Cataracts. Let’s find out more about these types of Diabetic Eye Disease and the treatments we offer.
Diabetic Retinopathy
Diabetic Retinopathy is one of the leading causes of blindness in the working population. The prevalence of Diabetic Retinopathy increases with duration of diabetes and nearly all patients with Type 1 and more than 60% with Type 2 diabetes develop some signs of Retinopathy. What is Diabetic Retinopathy The retina is the inner lining at the back of each eye. The retina senses light and turns it into signals that your brain decodes, so you can see the world around you. Damaged blood vessels can harm the retina, causing a disease called Diabetic Retinopathy. Damaged blood vessels can cause blurred, patchy vision and shapes floating in your field of vision.

Diabetic Macular Oedema (DMO)
Oedema means fluid retention. When leaky vessels cause fluid to build up in the macula, at the centre of the retina, it is known as Diabetic Macular Oedema. It is a complication of Diabetic Retinopathy and being diagnosed with DMO can be distressing and worrying but, with the right treatment, information and support, people can cope very well.
What is Diabetic Macular Oedema (DMO)?
The macula is the central part of the retina responsible for your central or ‘sharp’ vision. Diabetes can damage blood vessels in the macula which then leak and the surrounding retina can become swollen or ‘waterlogged’. This results in worsening of vision so that there is difficulty in tasks like reading, watching TV or recognizing faces.
The connection between Diabetes and Cataract
Elevated blood glucose causes the lens in the eye to swell. Over time, the lens starts to accumulate sorbitol (a type of sugar) which causes cloudiness of the lens and leads to cataract formation. The more severe your diabetic eye disease is, the higher the risk of getting cataracts.
3 Types of Treatment for Diabetic Eye Diseases
Laser Treatment
Laser treatment is used to treat new blood vessels at the back of the eyes in the advanced stages of Diabetic Retinopathy. This is done because the new blood vessels tend to be very weak and often cause bleeding into the eye. Treatment can help stabilize the changes in your eyes caused by your diabetes and stop your vision getting any worse, although it won’t usually improve your sight.
Eye Injections
In some cases of Diabetic Maculopathy, injections of a medicine called intravitreal injections may be given directly into your eyes to prevent new blood vessels forming at the back of the eyes. These can help stop the problems in your eyes getting worse, and may also lead to an improvement in your vision. The injections are usually given once a month to begin with. Once your vision starts to stabilise, they will be given less frequently and eventually stopped.
Eye Surgery
Surgery may be carried out to remove some of the vitreous humour from the eye. This is the transparent, jelly-like substance that fills the space behind the lens of the eye. The operation, known as Pars Plana Vitrectomy (PPV), may be needed if:
- A large amount of blood has collected in your eye.
- There’s extensive scar tissue that’s likely to cause, or has already caused, retinal detachment.
During the procedure, Dr Chetty will make a small incision in your eye before removing some of the vitreous humour, removing any scar tissue and using a laser to prevent a further deterioration in your vision. Vitreoretinal Surgery can be carried out under local or general anaesthetic depending on your risk profile.
PPV surgery can also be used to treat conditions such as retinal detachments, vitreous haemorrhage, endophthalmitis, and macular holes.